Posterior Reversible Encephalopathy Syndrome
Abstract
Introduction - Posterior reversible encephalopathy
syndrome (PRES) is a
clinicoradiologic entity occurring in varied
clinical setting and characterized by
headaches, confusion, visual disturbances,
seizures, and posterior transient
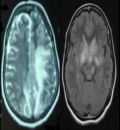
changes on neuroimaging. The radiological
features are often reported as demyelination
which confounds the diagnosis.
Observations - Of the 14 patients included
for the study, 13 (93 percent)
were females. The common symptom
being Headache in 13 (93 percent), Seizure
in 10 (71 percent), Visual disturbance
in 7 (50 percent), altered sensorium
in 7 (50 percent) and hypertension in
11 (78percent). On MRI the sites involved
were Occipital 13 (92 percent),
Parietal 9 (64 percent), frontal 4 (28 percent),
temporal 2 (14 percent), deep nuclei
2 (14 percent), cerebellum 1 (7 percent)
and brain stem 1 (7 percent). The
symptoms were reversible in 12 (86 percent)
patients, the remaining 2 (14 percent)
had complications of PRES with 1
(7 percent) having right occipital infarct
and 1 (7 percent)
right parietal hemorrhagic transformation.
Discussion -Acute rise in blood pressure is
one of the factors in the pathogenesis of
PRES, degree of raise in blood pressure
doesnt correlate with the clinical severity or
radiological manifestations. Pathophysiology
of PRES remains controversial with
two main hypotheses contradicting each
other. One being impaired cerebral autoregulation
leading to increased cerebral
blood flow (CBF) as noticed in severe hypertension,
whereas the other postulate is
endothelial dysfunction with cerebral hypoperfusion
as in cases with normal blood
pressure or on cytotoxic therapy. The common
final outcome in both is alteration in
cerebral perfusion with blood brain barrier
dysfunction causing vasogenic cerebral
edema. The common etiology of PRES in
this study was eclampsia, autoimmune disease,
renal disease and other causes.
Conclusion - PRES can manifest with
atypical features like normal blood pressure,
presence of MRI evidence of infarct
or hemorrhage. Clinical suspicion in appropriate
setting will lead to early diagnosis
and appropriate therapeutic intervention.
Reversibility of
the clinical and radiological abnormalities is
contingent on ealy treatment. On the contrary
when unrecognized, conversion to irreversible
cytotoxic edema may occur.
Full Text:
PDFReferences
Alexander M. McKinney, James Short
et al., Posterior Reversible Encephalopathy
Syndrome: Incidence of
Atypical Regions of Involvement and
Imaging Findings: AJR 2007; 189:904
–912. DOI:10.2214/AJR.07.2024
Hinchey J, Chaves C, Appignani B,
et al. A reversible posterior leukoencephalopathy
syndrome. N Engl J Med
; 334:494–500
Schwartz RB, Jones KM, Kalina P,
et al. Hypertensive encephalopathy:
findings on CT, MR imaging and
SPECT imaging in 14 cases. AJR 1992;
:379–383.
Schwartz RB, Bravo SM, Klufas RA, et al.
Cyclosporine neurotoxicity and its relationship
to hypertensive encephalopathy: CT and MR
findings in 16 cases. AJR 1995; 165:627–631
Schwartz RB, Feske SK, Polak JF, et al.
Preeclampsia–eclampsia: clinical and neuroradiographic
correlates and insights into the
athogenesis of hypertensive encephalopathy.
Radiology 2000; 217:371–376
Truwit CL, Denaro CP, Lake JR, et al. MR
imaging of reversible cyclosporin A-induced
neurotoxicity. Am J Neuroradiol 1991; 12:651
–659
Covarrubias DJ, Luetmer PH, Campeau
NG. Posterior reversible encephalopathy syndrome:
prognostic utility of quantitative diffusion-
- weighted MR images. Am J Neuroradiol
; 23:1038–1048
Casey SO, Sampaio RC, Michel E, et al.
Posterior reversible encephalopathy syndrome:
utility of fluid-attenuated inversion recovery
MR imaging in the detection of cortical and subcortical
lesions. Am J Neuroradiol 2000; 21:1199–1206
Jarosz JM, Howlett DC, Cox TC, et al. Cyclosporine-
related reversible posterior leukoencephalopathy:
MRI. Neuroradiology
; 39:711–715
Schwartz RB, Mulkern RV, Gudbjartsson
H, et al. Diffusion-weighted MR imaging in hypertensive
encephalopathy: clues to pathogenesis.
Am J Neuroradiol 1998; 19:859–862
Dillon WP, Rowley H. The reversible posterior
cerebral edema syndrome. Am J Neuroradiol
;19:591
Johansson B. The blood–brain barrier and
cerebral blood flow in acute hypertension.
Acta Med Scand Suppl 1983; 678:107–112
Tamaki K, Sadoshima S, Baumbach
GL, et al. Evidence that disruption
of the blood–brain barrier precedes reduction
in cerebral blood flow in hypertensive
encephalopathy. Hypertension
; 6[2 Pt 2]:I-75–I-81
MacKenzie ET, Strandgaard S,
Graham DI, et al. Effects of acutely induced
hypertension in cats on pial arteriolar
caliber, local cerebral blood flow,
and the blood–brain barrier. Circ Res
; 39:33–41
Trommer BL, Homer D, Mikhael
MA. Cerebral vasospasm and eclampsia.
Stroke 1988; 19:326–329
Ito T, Sakai T, Inagawa S, et al. MR
angiography of cerebral vasospasm in
preeclampsia. Am J Neuroradiol 1995;
:1344–1346
H. Ay, F. S. Buonanno, P. W.
Schaefer, et al, Utility of diffusionweighted
MRI Posterior leukoencephalopathy
without severe hypertension
: Neurology 1998;51;1369:
DOI 10.1212/WNL.51.5.1369
Belogolovkin V, Levine SR, Fields
MC, Stone JL (2006) Postpartum
eclampsia complicated by reversible
cerebral herniation. Obstet Gynecol
: 442–445
Lamy C, Mas JL (2001) [Reversible
posterior leukoencephalopathy. A new
syndrome or a new name for an old
syndrome?]. Presse Med 30: 915–920
S. Legriel, F. Pico, and E. Azoulay;
Understanding Posterior Reversible
Encephalopathy Syndrome;
Kazuma Nakagawa, Farzaneh A. Sorond,,
Allan H. Ropper.” Ultra-Early Magnetic
Resonance Imaging Findings of
Eclampsia “ Arch Neurol. 2008;65(7):974-
doi:10.1001/archneur.65.7.974.
Sakaharova AV. Regional characteristics
of the noradrenergic and cholinergic
innervation of the vessels of the brain
surface. Bull Eksp Biol Med 1980; 89:141-
Bartynski WS, Boardman JF (2007)
Distinct imaging patterns and lesion distribution
in posterior reversible encephalopathy
syndrome. AJNR Am J Neuroradiol 28:
–1327
Steinborn M, Leiz S, Rudisser K, Griebel
M, Harder T, Hahn H. CT and MRI in
haemolytic uraemic syndrome with central
nervous system involvement: distribution
of lesions and prognostic value of imaging
findings. Pediatr Radiol 2004; 34:805-810.
Wijdicks EF (2001) Neurotoxicity of
immunosuppressive drugs. Liver Transpl
: 937–942
Wang X, Lo EH (2003) Triggers and
mediators of hemorrhagic transformation
in cerebral ischemia. Mol Neurobiol 28:
–244
Szabo C (2005) Mechanisms of cell
necrosis. Crit Care Med 33 (12 Suppl):
S530–534
Allport JR, Ding H, Collins T, Gerritsen
ME, Luscinskas FW (1997) Endothelialdependent
mechanisms regulate leukocyte
transmigration: a process involving the
proteasome and disruption of the vascular
endothelial-cadherin complex at endothelial
cell-to-cell junctions. J Exp Med 186:
–527
Sweany JM, Bartynski WS, Boardman
JF. “Recurrent” posterior reversible
encephalopathy syndrome: report of 3
cases—PRES can strike twice! J Comput
Assist Tomogr 2007;31:148–56
Sibai BM, Sarinoglu C, Mercer BM.
Eclampsia. VII. Pregnancy outcome after
eclampsia and long-term prognosis.
Am J Obstet Gynecol 1992;166(6 Pt 1):
–61, discussion 1761–63..
Refbacks
- There are currently no refbacks.

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
An initiative of The Tamil Nadu Dr M.G.R. Medical University