A Study on Effect of Severity of Depression on Sleep Architecture in Diabetic Patients
Abstract
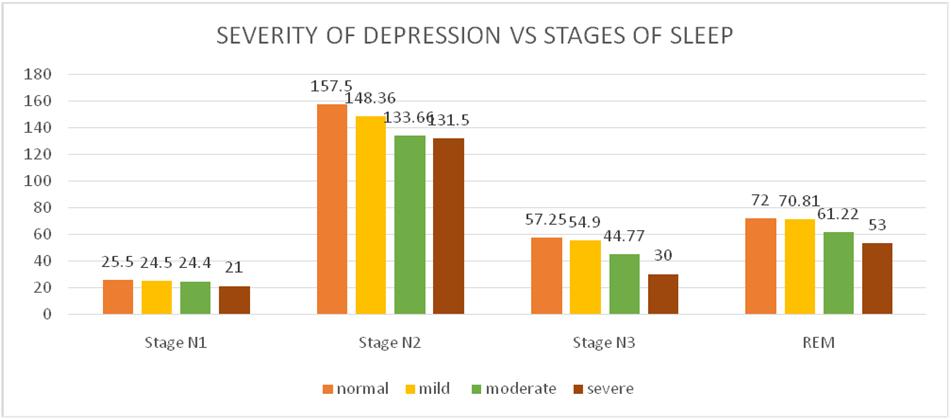
Background: Diabetes mellitus is one of the commonest health care problem in India with 13.5% prevalence. Sleep disturbances are common in type 2 Diabetes mellitus. Similarly the prevalence of depression in type 2 diabetes mellitus is 38.75%. Both depression and sleep disturbance are bi directionally related in diabetics and the severity of depression may have an effect on sleep architecture which is the basic hypothesis of our study. Objective: To evaluate the effect of severity of depression on sleep architecture in diabetics. Materials and Methods: A Total of 30 diabetic patients 40-60 years of age were enrolled. Digital Polysomnography was recorded in clinical Physiology research lab, Institute of Physiology and Experimental Medicine, Rajiv Gandhi Government General Hospital. HDRS (Hamilton depression rating scale) of each patient was calculated. Patients were grouped into various categories based on their severity of depression. They were then analysed in relation with sleep timing of different stages and also sleep latency and sleep efficiency. Results: Out of a total 30 patients 53.3% were males while the rest 46.7% were females. The mean age of the patients was 50.83± 5.38 years. Parameters were positively influenced by depression. As the severity of depression increases there is decrease in mean duration of each sleep stage and also the total sleep time and sleep efficiency and similarly there was an increase in sleep latency. Influence of severity of depression on all these parameters was statistically significant with P value less than 0.005. Conclusion: Severity of depression has a positive influence on the sleep architecture in diabetics.
Full Text:
PDFReferences
Resnick HE, Redline S, Shahar E, Gilpin A, Newman A, Walter R, Ewy GA, Howard BV, Punjabi NM: Diabetes and sleep disturbances: findings from the Sleep Heart Health Study. Diabetes Care 26:702–709,2003
Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, Patel S, Hu FB: A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 26:380–384, 2003
Kawakami N, Takatsuka N, Shimizu H, Ishibashi H: Depressive symptoms and occurrence of type 2 diabetes among Japanese men. Diabetes Care 22:1071–1076, 199
Luyster FS, Strollo PJ Jr., Zee PC, Walsh JK; Boards of Directors of the American Academy of Sleep Medicine and the Sleep Research Society. Sleep: A health imperative. Sleep 2012;35:727-34.
Hargens TA, Kaleth AS, Edwards ES, Butner KL. Association between sleep disorders, obesity, and exercise: A review. Nat Sci Sleep 2013;5:27-35.
Resnick HE, Redline S, Shahar E, Gilpin A, Newman A, Walter R, et al. Diabetes and sleep disturbances: Findings from the Sleep Heart Health Study. Diabetes Care 2003;26:702-9
Mooradian AD. Diabetic complications of the central nervous system. Endocr Rev 1988;9:346-56.
Zimmerman M Martinez JH Young D Chelminski I Dalrymple K. Severity classification on the Hamilton Depression Rating Scale. J Affect Disord 2013;150:384–388.
Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders: A meta-analysis. Arch Gen Psychiatry. 1992;49:651–68
Landolt HP, Gillin JC. Similar sleep EEG topography in middleaged depressed patients and healthy controls. Sleep. 2005;28:239–47.
Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression and anxiety. Sleep. 2005;28:1457–64.
Refbacks
- There are currently no refbacks.

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
An initiative of The Tamil Nadu Dr M.G.R. Medical University